Quality of life includes pleasure and play at any age.
“The World Health Organization defines sexual health as a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity.”
-CDC Website
It's been a minute or two since I posted to this blog. My attention has been focused on presenting some webinars, one of which was none other than what you're reading about now! So, if you saw the webinar, here are many (not all) of my notes.
We’re going to start with a little bit of information and advocacy stuff. Another life ago–about 20 years– I was in massage school studying to be a Licensed Massage Therapist long before getting my master’s in counseling. That license lapsed about a decade ago, but I still carry with me a lot of what I learned. One of those things is the “pelvic clock.” If you’re not already familiar, it's an exercise involving rotation of the hips to help people develop core strength and movement to address low back and hip pain. We were advised that the elderly were seldom fans of this movement, sadly, because it reminded them of hopeless, long abandoned sexual feelings. At 20-something I was able to register this information academically and clinically. As I note my own aging and the aging around me, it hits more personally now. It makes me sad and angry that people are compelled to abandon this part of themselves.
According to recent Census Bureau estimates, there are over 50 million senior citizens in the U.S. That’s over 16% of the population that's 65 years old and up. AARP’s website reports there are almost 110 million people over 50. That's a lot of people for whom a big piece of their quality of life may slip through the cracks. We naturally may crave and have the capacity to enjoy sex and physical intimacy throughout our life– not just in our younger, more gravity-defying, juicier years.
“Positive and passionate romantic relationships are not only fulfilling at any age; they've been associated with real
health benefits. These include lower stress levels, better healing after surgery, healthier behaviors, and even a longer lifespan. Intimacy has even been found to ward off
depression. Physical affection has been linked to lower resting blood pressure and
higher levels of oxytocin, a feel-good hormone.”
-National Council on Aging
According to a 2018 poll by University of Michigan Health, about two thirds of older adults are at least interested in sex, regardless of whether or not they're actually engaging in any kind of sexual behavior.
Compare that to the mere 17% of those same study respondents that actually talked to their doctor about it, and most of those few had to bring it up themselves… which tell us that the sexual potential and the intimacy needs of older folx are getting overlooked or dismissed (and don't get me started on the disparities for older AND younger folx in the sexual and gender minority). On the doc side, Seniors Lifestyle Magazine postulates that maybe it’s based on ill-advised assumptions by the doctor about who has sex in our culture and who doesn’t. Or maybe the doctors aren’t up to snuff when it comes to treating sexual concerns and goals for older folx. Maybe they assume the patient will bring it up if they need to. Maybe it gets swept aside for other issues that may or may not be more pressing. It could also be the cultural taboo around sex that keeps doctors and patients from bringing it up. Or it could be myths about it that patients have settled into believing (like sex is only for the young), or maybe they just don’t realize their sexual behaviors could be better, safer, and more fulfilling. So, it doesn’t get brought up, and it doesn’t just keep seniors from getting support in the sex and intimacy domain. It also puts seniors at risk for neglect of other underlying medical conditions – sudden loss of arousal could be related to things like heart disease, hypertension, high cholesterol, or diabetes.
I see no compelling justification for the omission of sex conversations in the doctor’s office. I see plenty of compelling reasons to advocate for them.
- It normalizes and validates what is already normal.
- It opens the door for myth-busting and education. Yes, old people like sex also, and yes, old people also benefit from safe sex information! (STI rates among the elderly have skyrocketed in recent years.)
- It increases the chance of catching underlying and possible urgent medical issues.
- It empowers older people to improve their quality of life, both physically and emotionally.
On that last note, imagine how much easier could it be for us, as we age, to stay connected with our capacity for sensuality and the related health, wellness, and quality of life that comes with it, if sex were validated and addressed by the systems in place around us. And let’s take those conversations and that education home with us. We can take it home for our own self care, and pleasure and we can take it home to share with our partners and lovers.
Just like in so many other domains, representation and acknowledgement matter.
With that in mind, as we pivot from advocacy to the experience of sex after menopause, I want to note that these are generalized numbers and concepts gleaned from research that is overwhelmingly based on the cisgender experience of menopause, but the perspective of gender variant folx should not be overlooked or excluded.
Let's address the common vocabulary. Ciswomen are the default, the assumed, when it comes to menopause, and all our quotes from the reading and research I found reflect the cisnormative world we live in, referring to "women." We won’t get deep into gender diversity today– check out the Gender Diversity in the Family System webinar from January 6, 2023 for that– but I do want to underscore that gender diversity is as old as the human race. So, while it may be relatively uncommon when we look at rates of occurrence in the general population, it is definitely a normal part of human existence.
- There are about 1.3 million adults (0.5%) and about 300,000 youth ages 13 to 17 in the U.S. (1.4%) that identify as transgender, but gender diversity occurs throughout all ages, races, religions, ethnic, and cultural domains.
If you're cisgender, you might be asking yourself right now, what does this have to do with menopause? Transphobia, trans myths, and trans erasure on the systemic side, and gender dysphoria on the individual side have very real consequences for gender variant folx, including support (or lack thereof) when it comes to reproductive health, sexual health, and aging– exactly the intersecting domains we’re looking at.
A third of participants from the U.S. Transgender Survey reported at least one bad experience with a healthcare provider related to their gender identity. These experiences lead to not just subpar or denial of care, but also AVOIDANCE of care because of a realistic fear of not being treated in a professional, informed, or compassionate fashion.
Menopause doesn’t just affect ciswomen. Anyone who has at least one ovary, is not on masculinizing hormones, and reaches the age of menopause will feel its symptoms just like a cisgender woman, which can vary widely from person to person. Just like ciswomen, transgender and gender nonconforming (TGNC) people need clarity on all aspects of reproductive and hormonal health, but they are often left out of the conversation, so this blog is here to invite them in.
One of the very first things I try to do is use inclusive language. The quotes here lack that because of the systemic defaults already noted, but I’m going to do my best to stay mindful of it, using the word people in place of the literature’s use of the word “women.” If you catch me using exclusive language, I encourage you to shoot me a message point it out so I can fix it!
"The sexuality of older women is influenced by many factors, including general physical and mental well-being, quality of relationship, life situation, marriage status, menopausal status, education, social class, stressors, and self perception."
(Lochlainn and Kenny, 2013)
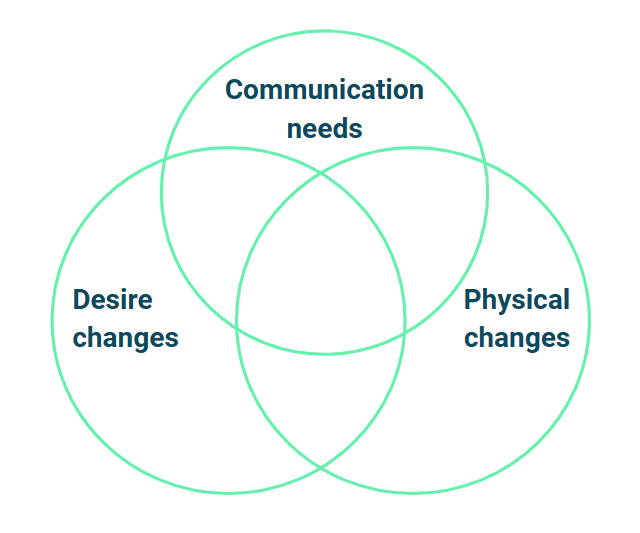
As you can see, there are a lot of overlapping domains when it comes to someone’s sex life after menopause.
Courtesy of Wichita’s Center for Women’s Health, a few quick myths that we’re going to dispel include:
- Menopause ends your desire for sex.
- Menopause ends sexual pleasure.
- There’s no way to spice up your sex life after menopause.
As we’ll get into, desire can decrease as a result of menopause. That part is true. Like so many myths, this one is based on partial truth. Whether the decrease is for psychological or physical reasons or both depends on the person, but that’s not the end of the story. With the right support and insights, desire can be maintained and arousal tapped into.
It’s also true that physical changes to our bodies and the emotional responses to those changes can impact our ability to feel pleasure, but again, that’s not the end of the story either.
So, the first 2 myths are partly true but overstated; any Politifact fans? Not quite pants on fire, but still mostly false.
As for no way to spice up your sex life? That’s just pants-on-fire silly, and we’ll talk about that too.
A quick internet search for “why talk to partner about menopause” had a lot of really helpful results, and it also had big, bold recommended “similar search” results like:
- “Can marriage survive menopause?”
- “How do you deal with a menopausal wife?”
- “My menopause wife hates me?”
- “Can menopause cause a sexless marriage?”
It’s just a part of life, and it doesn’t have to be devastating.
So, what exactly is menopause?
In the US it’s officially just one day– the very last day of the very last menstrual cycle. Anything before that is perimenopausal, and anything officially after is postmenopausal. Unofficially, according to Jen Gunter (again), it’s “puberty in reverse,” when people who once ovulated can no longer ovulate. That means no more eggs. No more periods. No more chance of pregnancy no matter how many sperm may or may not swim their way through that canal.
Menopause can occur naturally, or it can be the result of surgery like a hysterectomy, or it can be the result of medical treatment like chemotherapy (That, my friends, is why I am 43 years old and haven’t had a period in 4 years). Symptoms of menopause can also occur when transfolx get on masculinizing hormones.
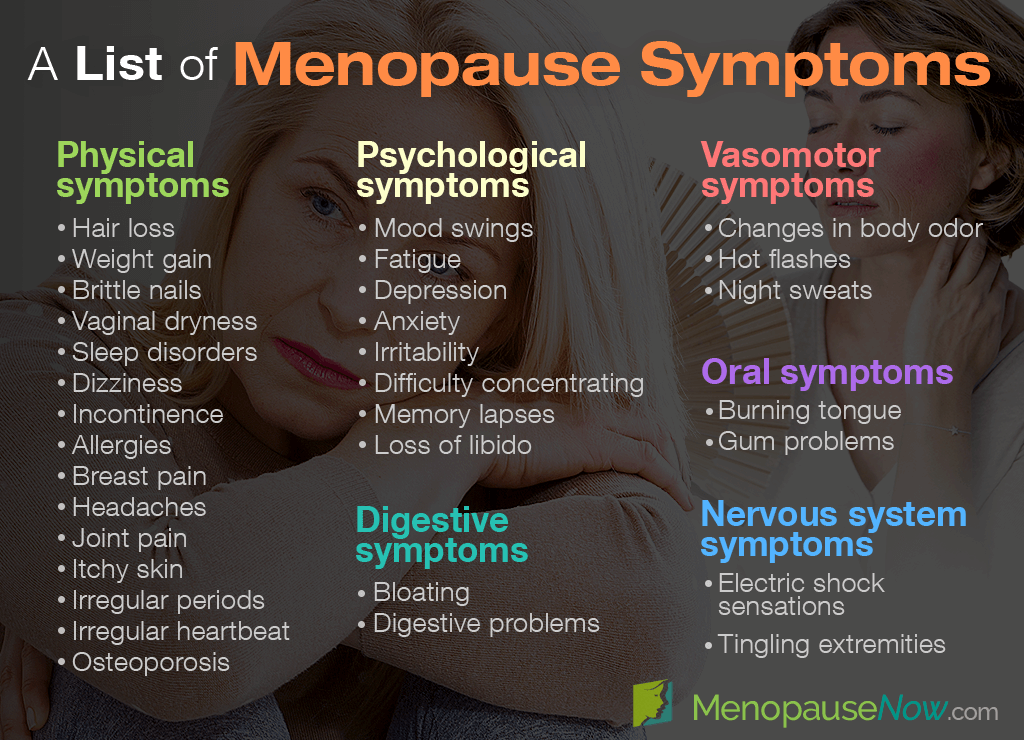
No period? Honestly, no complaints there from me. But what else? What are the symptoms?
So, sure. It’s not a walk in the park on a perfect sunny day. There are challenges that come with this transition. People may experience anywhere from none to all of these, each with its own spectrum of severity.
One more that a lot of people note that didn’t make it to this list for some reason is an increase in facial hair to go with the decrease in hair elsewhere.
Society says this is when we start spending our paychecks on wigs and depilatories!
To be fair, a lot of these are temporary, lasting through perimenopause only, but others do stick around into postmenopause, and they do make themselves quite comfortable for the duration.
- Difficulty with arousal
- Decreased desire
- Vaginal dryness
- Thinner vaginal skin
- Weight gain
- Vaginal pain
- Difficulty with orgasm
- Decreased clitoral sensitivity
I know. None of this is making you feel any better yet, and we live an average of 30 more years after menopause. That’s a lot of life and a lot of sacrifice if you’re tempted to give up on sex and your sensuality because of an ageist lens and because it’s no longer as easy or automatic as it used to be, but look at it this way: I can’t effortlessly run in endless circles like I did on the playground as a kid. On top of that, because of menopause, I’m not even remotely close to the "athlete" (I use this term loosely) that I was just 5 years ago, but I still find joy in movement and exercise. I appreciate their benefits, and I plan to KEEP movement and exercise as part of my life. How they are part of my life is just different now and the changes are going to keep happening over the years to come. There’s some
grief around that, and that’s ok.
Let’s look at that word GRIEF. We all know it doesn’t just apply to literal death. We experience all kinds of existential and ambiguous losses over the course of our lives, and the changing nature of our bodies and sex lives is one of them.
So, we can acknowledge that menopausal changes can be a big challenge and they do merit adjustment in how we approach sex, so let's bring this back around to having difficult, maybe awkward conversations with our partners.
What’s hard on one person is almost inevitably hard on the system. Without education, understanding, and communication, sensuality, intimacy, and relationships can and do fall apart, just like the Google searches implied.
One place we run into this is when we try to ignore or avoid our changing bodies and then neglect to communicate about those changes or that avoidance with our partner. Just like the stories so many of us may have heard or experienced where cishet women personalize the erectile dysfunction of their partner as something wrong or insufficient with themselves, those partners without an understanding of the changes that happen with menopause may likewise be tempted to perceive the lack of lubrication, lower desire, and maybe even pain during sex as a failure on their own part. Another version of that could be one, the other, or both partners believing the menopausal individual is just “broken.”
Without an informed, vulnerable conversation about what the body just simply does (IT’S NOT BROKEN), a wedge gets driven between people and desire is driven even further underground because of insecurity and stress. Not understanding our bodies, expecting them to function the same at 50 as they did at 25 does us all a disservice.
With education, understanding, and communication, on the other hand, we get to discover that we still can enjoy sex, sensuality, and physical intimacy into old age.
And this is when we start getting into the good news. Just reading this article means you are already addressing and looking to help other people address one of the hardest of what I see as
three interlocking parts to cultivating a sex life with longevity: Communication needs. The other two parts are the tasks of addressing desire (emotional) changes and physical (physiological) changes.
Since we’ve knocked out communication already, let’s move on to the other two domains, starting with desire. It’s generally understood as emotionally wanting sex; not to be confused for arousal, which is the body’s physiological response to sex. Of course, ideally there’s going to be plenty of overlap between the two, but that doesn’t always happen, especially as we get older. This disconnect between arousal and desire is called arousal
non-concordance, and it’s not just for old folks. In a nutshell, we can have desire without physical arousal, and we can also have physical arousal WITHOUT desire. Side note: that’s a really important fact when we start navigating the world of sexual trauma, but that’s a conversation for another day.
Things that negatively impact desire include (but aren’t necessarily limited to):
- Aging (of course; that’s what we’re talking about today!)
- Settled, stable relationships
- Any number of “brakes”
Anybody surprised by stable relationships?
Emily Nagoski’s book,
Come as You Are, describes our sexual nature through the concept of accelerator and brakes that are influenced by both external and internal experiences. External includes anything that could be going on in our life or around us, internal is all the thoughts, feelings, and beliefs ABOUT all the things that are going on in our life and around us AND about OURSELVES. As you might imagine, accelerator implies approach and brakes suggests slow down or stop.
All three of these things overlap. As we age we are more likely to settle into relationships, and as we age and settle into relationships we are also more likely to experience an increase in both our internally and externally influenced brakes. Job, kids, life expectations, ADULTING, body changes, values shifts, politics, etc.
While time management and work/life balance are definitely important when it comes to managing the brakes, and I definitely want you to keep that in mind when it comes to desire, we’re mostly going to focus on addressing the internally oriented stuff here. For starters, we live in a culture that tends to sexually value youth and devalue the older experience. Joan Price, author of
Naked at Our Age, offers this frame for appreciating and believing in our own sexiness at any age: Each day is the youngest we’ll ever be again, and besides, most of us were also pretty damn hard on ourselves in our 20s. A negative self-image has been documented as one of the biggest barriers to desire that ciswomen experience, and it’s no doubt problematic among other populations. In order to experience desire, we also have to believe we are desirable, just as we are… and with maybe a little optional leather, lace, and tassels.
There was a viral TikTok a while back. I can go down an embarrassingly long TikTok rabbit hole.
The original sound came from a guy asking someone on the street to rate themself from 1-10. People from both within and outside the conventional beauty standard borrowed that sound and made it their own. “I’m a 10.” Unflinching, beautifully bold and confident: I’M A TEN.
This
clip is over 11 minutes long, and I recognize that these folx are mostly young and white and femme presenting, but it’s the only compilation clip I could find and I’m not tech savvy enough to make my own!
Every time my 76 year old mother (who is, of course, a stunning 10, mind you) starts bashing herself, I like to remind her of those videos, but I don’t think she appreciates the wind taken out of her self-deprecating humor sails. When I was relatively younger, any time someone would take a picture of us all, she’d tell my brother and me that one of us needed to pull on the skin on the back of her neck to give her a photographic “face lift.” These were the days before filters, you see. We also used to joke that it’s much better to lie about being older than younger as we age. If we say we’re younger, people are going to wonder what kind of tornado hit that made us look so raggedy at such a young age. If we say we’re older than we really are, we get to hear stunned remarks about how great and young we look. It’s funny, and I chuckle, but the underlying beliefs that we are unworthy and unattractive and definitely not sexy as we age are still damaging. So, fuck that. I’m a 10. You’re a 10. We’re all 10s!
I love those clips. They are a fabulous reminder to practice self love when the inner critic starts telling us we’re supposed to be younger, juicier, smoother, firmer, rounder, and wetter.
In addition to reminding us about our relative youth, the book
Naked at Our Age also says that in order to maintain a satisfying intimate life into old age, we need two senses: “common sense and a sense of adventure.” These senses fit right in with our need to address communication, desire, and physical changes. And it occurs to me that these 2 senses are also not entirely distinct from one another. In a culture where the very topic of real sexual connection is taboo (insert cultural cognitive dissonance and double standards between cismen and everyone else here), the common sense concepts of believing in, prioritizing, and being intentional about our sexuality is a pretty radical, adventurous move.
So, our first radical, common sense strategy to experiencing desire is our own mind and body self care, recognizing and nurturing our own desirability. Take care of yourself. Listen to and take care of your body and your mind. I’m bringing body into this because your head is stuck to your body just like mine. Whatever is going on below the neck, there’s a mental/emotional impact. Whatever is going on above the neck, there’s a bodily impact. So, taking care of one can also help the other. While sex and exercise and nutrition could be a whole other presentation itself, suffice it to say that a healthy (enough) lifestyle and CONFIDENCE are related, contributing factors among those who report satisfying sex lives into old age.
Common sense says that if you want sex to be a part of your life, create a welcoming physical and emotional context for it. When sex and intimacy are at risk of being left behind despite a fundamental belief in their importance, maintaining them has to become a deliberate, mindful endeavor.
Part of taking care of our body and mind at every stage, and maintaining a connection to our sexual selves, becomes a matter of recognizing and accepting what doesn’t work anymore while also shifting focus to what can and does work
(thank you, 63 year old
Nina Hartley, for that bit). We can accelerate. It just looks different, requires curiosity and patience, and we need to make sure we’re finding ways to ease up on the brakes.
One way to do that? Schedule your sexy time. Ew, what? Sex is supposed to be spontaneous! Scheduling makes it sound like an office meeting, like a duty or an obligation. Something that you check off your to-do list. Gross.
Scheduling opens opportunity to prioritize what we value– ourselves, our sensuality, our partner, their sensuality.
Esther Perel notes that “Unconditional love does not drive unconditional want” and we often “have smothered sizzle with affection, leaving it no way to ignite.”
In long term relationships, we can get really comfortable. On average it takes about 6 months to 3 years for that initial ripe, fertile ground for spontaneous desire for one another to more or less dry up. We start to take each other for granted to some extent, and that’s actually a good thing. I love knowing that my husband of 10 years and I still love each other when our breath stinks, we’re bloated, our noses are running, and there are dinner stains on our PJs that we haven’t changed out of in 3 days. It’s a different and secure kind of love than what we may have had in the past, and it’s definitely not sexy. At least not for us. We “have smothered sizzle with affection, leaving it no way to ignite.” We’re not going to get an itch for amazing spontaneous sex in this context (nor in the context of busy work days and all the other life brakes that we juggle from day to day), so if we’re going to invite sex into our relationship, we have to carve out time. We have to schedule. And I want you to check how you’re conceptualizing scheduling.
It could be 30 minutes.
– Babe, I’m going to take a shower and throw on that outfit that you like. How about we meet upstairs in 30 minutes?
It could be 10 days.
– Babe, as soon as I get this work project finished I want to make YOU my project. Let’s put the world on pause on (set the date and time and do what you need to do to make space for yourselves).
And when you meet upstairs or after the project is done, I invite you to also leave any expectations about what pleasure and sex SHOULD be at the door. Instead, adopt a curious, playful concept of what it IS in the present moment, right now (Well, not like NOW now, but on your sexy time date!)
Maybe this time it’s just cuddling and talking. Maybe this time it’s making out like teenagers at the movie theater in the 80s. Maybe it’s just caressing and observing and appreciating all the nuances of each other’s body. Or MAYBE this time it’s the most mind-blowing sexual experience you’ve ever had, complete with simultaneous, explosive, and multiple orgasms you’ve EVER had in ALL your life. Maybe it’s a little bit of all of it. My point is,
the performative pressure we put on ourselves and our bodies, and the unrealistic expectations that we’ve internalized from both sexual myths and media don’t do us any favors, and actually create far more of a barrier to attuned, physiological, emotional, and orgasmic connection.
Use planned time for sex as an opportunity to build excitement and anticipation.
In the time between plan and action, flirt, love and support each other in meaningful ways, build the excitement and anticipation.
It’s not that easy, though,
we say. We can’t just push a button anymore and feel desire, and we’re right.
That’s one reason we leave our expectations at the door. Our purpose is to enjoy one another and create the context for pleasurable things to take place.
But also, if you’re not in the mood and you don’t WANT to be in the mood, that’s cool. Carry on. Not everyone wants sex and not everyone wants to want sex.
But, if sex IS something you want and IS something you want to want, an important thing to understand is that as we age arousal and desire more commonly follow action rather than the other way around. Our desire becomes more RESPONSIVE rather than spontaneous, so we have to cultivate the context for it. If we wish we were in the mood, we are tasked with doing something to GET in the mood and to lean into that responsive desire.
From there, that’s where the sense of adventure really gets to come out and play. Now that we’ve shown up to play and practiced radical acceptance that sex and desire don’t work like they did in our younger years or earlier in the relationship, we open space to be curious, adventurous, experimental, and COMMUNCATIVE about what works for us NOW. We get to explore this new era in our sexual development.
This adventure can be as vanilla or as spicy as we see fit. Old sex can’t be spicy? Puh-SHAH. Intimacy and sex get to be defined and redefined to the limits of our imaginations and can include (if we want) all kinds of additional resources. Once again, common sense and sense of adventure overlap. Common sense says to acknowledge your body’s changes; sense of adventure invites you to have fun with the tools and resources and supports at your disposal.
Modern times come with effective modern solutions to some age-old biological problems for the postmenopausal human. We experience decreased lubrication and dryness, decreased elasticity, thinner more fragile skin that’s more susceptible to tearing, increased potential for pain, and decreased clitoral sensitivity. Fortunately, the world we live in today offers us an array of genital moisturizers and personal lubricants that can be incorporated into self care routines and sexual play to help keep touch pleasurable and the skin of the vulva and vagina healthy.
It could take some trial and error to find a lube that you like, but it can be a game changer once you do. Additional tools can include pillows, props, swings and sex furniture, different positions, vibrators, floggers, feathers, and any number of other sexual aids to help find what works and what you like as the years advance and needs change. Another tool, but arguably a more challenging one to apply, is a reconceptualization of our definition of sex and intimacy. Like we mentioned earlier, pressure and expectations based on myths and youth don’t do us any favors. Curiosity, innovation, and that sense of adventure WILL. And, yes, I will be repeating these things today. Hi, my name is Broken Record.
We can also talk to our doctor, hopefully. If you can’t talk to your doctor about this stuff, I encourage you to find a new doctor. Our doctors should be able to advise about possible hormonal options and/or pelvic floor physical therapy. Vaginal dilators are also worth discussing to help vaginal musculature relax for folx who want and are struggling with penetrative sex.
Of course, age-old common-sense solutions to age-old problems also have their place. To encourage circulation and maintain sensitivity and muscle tone (in other words easier orgasm and capacity for pleasure), vaginal massage, clitoral stimulation, kegel exercises, and regular orgasm (with a partner or without) don’t necessarily require any kind of tools or professional assistance. Although, vibrators have been noted as highly useful for vulva owners to consistently and quickly achieve orgasm.
A Word on Numbing Cream
My mom didn’t talk about her own experience when I mentioned this research endeavor to her, but she did chuckle and tell me that someone else in our family was prescribed numbing cream to address her experience with painful sex. While her experience was probably 25+ years ago, it’s still not necessarily unheard of for people to receive this type of treatment.
Talk to your doctor about what could work for you, but it may not be ideal because…
- It can increase risk of tearing and injury (because you can't feel damage as it happens).
- It doesn’t address the underlying cause/causes.
- It limits pleasurable sensations also, not just painful sensations.
- It could also impact partner sensation and pleasure.
BUT, it’s possible that using it AFTER could be helpful if there is residual pain or discomfort.
And What About Medications?
"Addressing the suspected underlying contributing factors for HSDD is often the best approach, focusing first on the factors that are particularly stressful to the woman."
- University of Colorado Ob-Gyn
Let it be known that I AM NOT A DOCTOR OR MEDICAL PROFESSIONAL. This is just information that I dug up from those that ARE medical professionals that have posted on the internet.
Bremelanotide (Vyleesi)
- Injection as needed; no more than 8 doses a month or 1 dose in 24 hours
- FDA approved for premenopausal female sexual interest/arousal disorder (FSAID)
- Potential side effects: temporary high blood pressure, nausea, flushing, injection site reactions, headache, vomiting, gum and skin darkening (particularly in the face and the breasts)
Flibanserin (Addyi)
- Daily pill at bedtime
- FDA approved for premenopausal female sexual interest/arousal disorder (FSAID)
- Additional studies indicate
similar effectiveness and tolerance in postmenopausal study participants.
- Potential side effects: dizziness, somnolence, nausea, fatigue, insomnia, dry mouth, and severe hypotension (low blood pressure) and syncope (loss of consciousness) when taken with alcohol (and other contraindicated medications)
"to date, the observed effects of flibanserin and other new drugs seem limited in terms of clinical significance"
(Both, 2017)
Off Label Medications
“All medication options require monitoring of the patient, as risk assessments of these off-label drugs for HSSD patients has not been fully explored.”
- University of Colorado Ob-Gyn
- Testosterone
- Bupropion
- Buspirone
Again, TALK TO YOUR DOCTOR. It may or may not work, and the side effects may not be worth it.
To sum up, with education, radical acceptance, and bold communication– with our common sense and our sense of adventure– we get to reconceptualize what it means to be sexy and to have intimacy. We get to remain open to our desirability and desire, our sensuality, and our pleasure. If you want a sexual life as you age (it’s fair to say that not everyone does), set yourself up for it. Invite it in, deliberately, patiently, and with curiosity, kindness, and joy. You’re still a 10.
Resource link